The United States is facing a sharp surge in drug-resistant bacterial infections, particularly those carrying the New Delhi metallo-β-lactamase (NDM) gene. Between 2019 and 2023, cases increased by nearly 70%, posing a serious challenge for public health authorities. The trend reflects a broader global crisis of antimicrobial resistance (AMR), which threatens to make common infections untreatable.
Current Situation in the U.S.
According to data from 29 states, 4,341 carbapenem-resistant infections were reported in 2023. Alarmingly, 1,831 cases involved bacteria carrying the NDM gene, which can resist carbapenems—the last line of defence antibiotics. The rise in NDM cases alone has spiked 460% since 2019. Experts warn that many carriers remain undetected, heightening the risk of community spread.
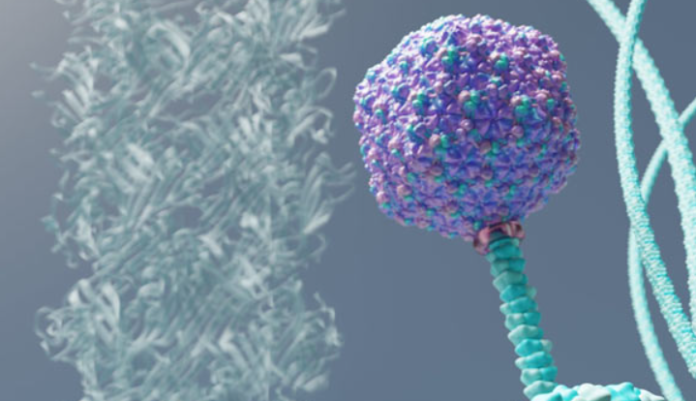
How Bacteria Develop Resistance
Bacteria adapt to antibiotics through genetic changes and survival mechanisms. Misuse of antibiotics—such as incomplete treatment courses or unnecessary prescriptions—accelerates this process. Resistant strains not only survive but also pass on resistance genes, creating “superbugs” that are increasingly hard to treat.
Role of the COVID-19 Pandemic
The COVID-19 pandemic played a significant role in worsening antimicrobial resistance. Over-prescription of antibiotics during COVID-19 waves, prolonged hospital stays, and overburdened healthcare systems contributed to the spread of resistant strains. Experts caution that the true extent may be underreported due to gaps in testing, especially in large states like California and New York.
Symptoms and Risks
Carbapenem-resistant infections often resemble common bacterial illnesses, delaying detection.
- Urinary Tract Infections (UTIs): burning sensation, cloudy urine
- Bloodstream Infections: fever, chills, low blood pressure
- Pneumonia: cough, chest pain, shortness of breath
Early diagnosis and specialized treatment are critical for survival.
Global Outlook on NDM Bacteria
- South Asia (India, Pakistan): Highest prevalence due to antibiotic misuse and overcrowded hospitals
- Europe: Southern Europe reports higher rates than northern countries with stronger infection control
- Africa & Latin America: Weak health systems and sanitation gaps worsen spread
- Travel & Trade: NDM bacteria spread easily via international travel, food, and livestock
Challenges Ahead
The U.S. and global health systems face major obstacles:
- Limited diagnostic capacity for resistant strains
- Weak antibiotic regulations in many regions
- Poor public awareness of AMR risks
Experts stress the need for infection prevention, strict antibiotic stewardship, stronger surveillance, and global cooperation to contain the crisis before it escalates further.

